Research
Dissecting the biology of metastasis
The vast majority of cancer-related deaths are due to the ability of cancer cells to spread away from their primary location, leading to vascular challenges and metastasis formation (external page WHO). This accounts for more than 7 million deaths each year worldwide, and little is known about how to block metastatic progression in patients.
Our laboratory is interested in understanding the fundamental molecular mechanisms that drive cancer and its metastatic progression, with a particular focus on the analysis of circulating tumor cells. In our studies, we use a combination of molecular biology, next-generation sequencing, computational biology, microfluidic and robotic technologies, patient samples, in vivo models, genetic engineering, CRISPR screens and drug screens to better understand the biology and vulnerabilities of aggressive cancers. We collaborate actively with a number of academic research groups, hospitals, and healthcare companies throughout the world, striving to identify novel metastasis-relevant therapeutic opportunities to fight against the metastatic spread of cancer.
Circulating tumor cells and their clusters
Cancer cells that leave the primary tumor site and are transported through the circulation to distant organs are referred to as circulating tumor cells (CTCs). While CTCs are extraordinarily rare in the peripheral circulation of patients with cancer (approximately one CTC per billion normal blood cells), they hold the key to dissecting fundamental aspects of how metastasis occurs. We isolate CTC from the blood of cancer patients using specialized microfluidic technologies, and interrogate them at the molecular and functional level to uncover their fundamental biological properties and vulnerabilities.
For example, we recently discovered a major role for CTC clusters (aggregates of cancer cells in circulation) in the metastatic process. We found that CTC clusters are derivatives of hypoxic tumor areas and are characterized by hypomethylation of the binding sites for transcription factors that simultaneously regulate stemness and proliferation, corresponding to a highly metastasis-prone phenotype (external page Aceto et al., Cell, 2014; external page Gkountela et al, Cell, 2019; external page Donato et al., Cell Rep, 2020) (Fig. 1).
In a prospective rapid autopsy study, we uncovered peri-mortem surges in CTC clusters, alongside vascular infiltration of tumor cells and occlusion of major blood vessels – events that strongly associate with reduced overall survival in patients with carcinoma (external page Newcomer et al., Nature Medicine, 2025). This, together with positive results from our proof-of-mechanism, prospective interventional study that demonstrated CTC clusters disruption upon inhibition of the NaK ATPase in breast cancer patients (external page Kurzeder et al., Nature Medicine, 2025), suggests that targeting CTC clusters might be a valuable therapeutic strategy for patients with aggressive cancers.
We also discovered a high degree of heterogeneity within individual CTC clusters. Not only can they carry more than one tumor subclone at the same time (external page Aceto et al., Cell, 2014; external page Gremmelspacher et al., Nature Genetics, 2025), but they can also occur as heterotypic units, often associated with neutrophils that enhance their proliferative and metastasis-forming capabilities (external page Szczerba et al., Nature, 2019).
Together, our recent investigations allowed us to better understand some of the key properties of the metastatic process, including the formation of homotypic and heterotypic CTC clusters, as well as some of their driving principles and vulnerabilities.
Timing and cues to circulating tumor cells intravasation
We are interested in understanding signals that dictate the intravasation of cancer cells in the bloodstream, as well as properties that define their ability to metastasize to various organs. A better understanding of these features may enable future therapeutic opportunities.
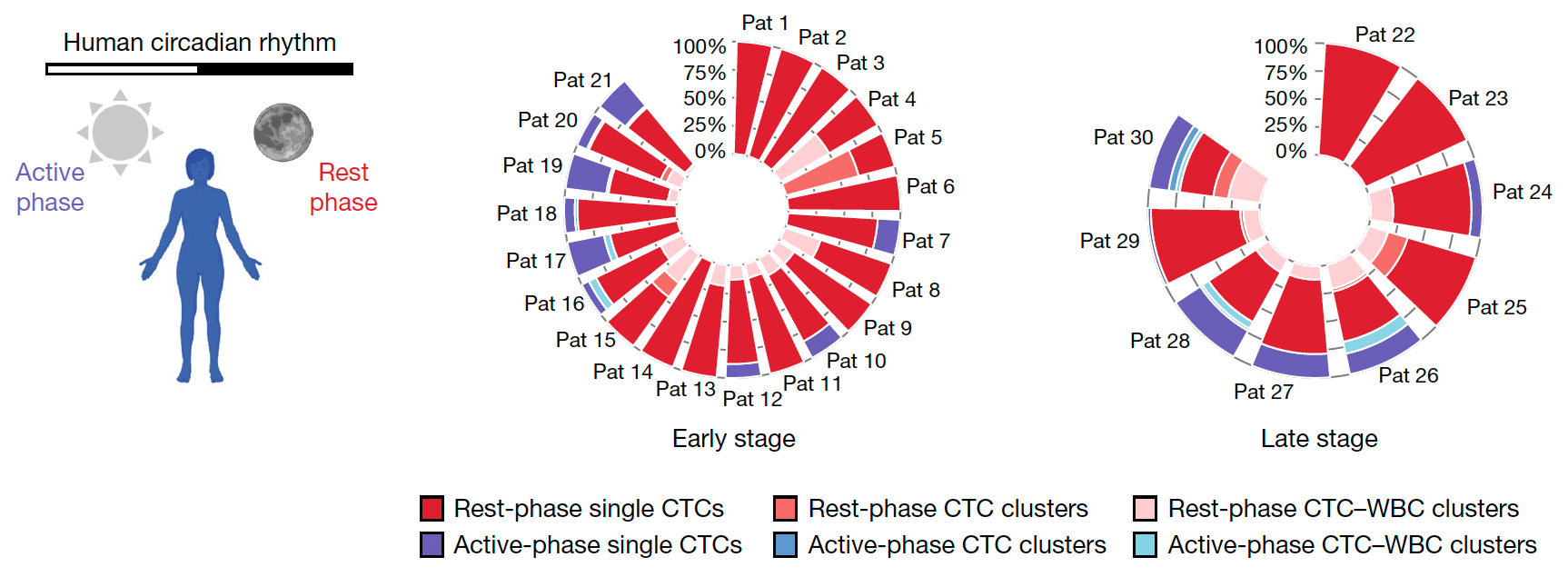
We discovered a key role of the circadian rhythm in regulating timing of CTC intravasation. Particularly, we observed that most CTC are generated during the rest phase (i.e. sleep) of breast cancer patients and mouse models, and that the majority of successful metastatic events can be ascribed to the same period. This occurs through the action of circadian rhythm-regulated hormones, which simultaneously regulate cancer cells proliferation and invasion into the bloodstream, yet in a time-dependent fashion (external page Diamantopoulou et al., Nature, 2022) (Fig. 2).
Further, with a genome-wide CRISPR screen in vivo using patient-derived CTC xenografts, we improved our understanding of genes that regulate specific aspects of the metastatic cascade. These include genes that promote CTC intravasation and colonization to specific distant sites, such as bone, brain and liver (external page Scheidmann et al., Cancer Res, 2022). We also generated StealTHY, a platform that enables immune-stealth CRISPR-based experiments in immunocompetent contexts, including humanized models. This has enabled the identification of (previously concealed) metastasis-relevant genes as well as genes that are critical in tumor-immune interactions (external page Saini et al., Cell, 2025).
Altogether, these findings allow us to plan future metastasis investigations in a time-controlled fashion and in immunocompetent contexts, considering the role of the circadian rhythm in this process and well as the action of specific cancer-relevant genes in vivo.
Video summaries of our main discoveries, in a nutshell
Research in our lab is focused on improving our understanding of the metastatic process. Our key discoveries are summarized below, stay tuned for more…